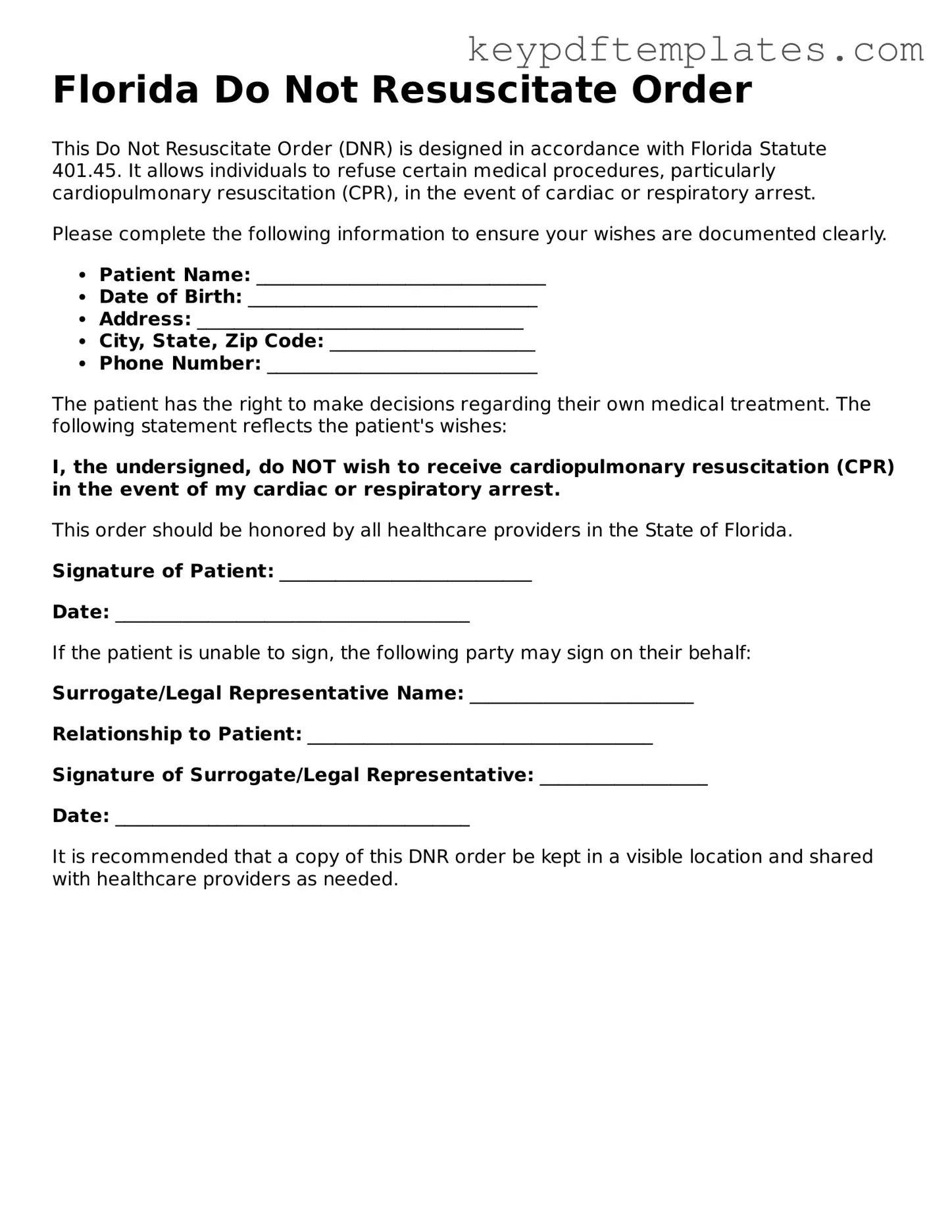
Legal Do Not Resuscitate Order Document for the State of Florida
Key takeaways
Understanding the Florida Do Not Resuscitate Order (DNRO) form is crucial for ensuring that individuals' healthcare preferences are honored. Here are some key takeaways regarding its use:
- Eligibility: The DNRO is intended for adults who wish to refuse cardiopulmonary resuscitation (CPR) in the event of cardiac arrest.
- Completion: The form must be completed by a qualified physician who is familiar with the patient's medical history and wishes.
- Signature Requirement: The DNRO must be signed by both the patient and the physician to be considered valid.
- Distribution: Once completed, copies of the DNRO should be distributed to all relevant healthcare providers and kept in accessible locations.
- Revocation: Patients have the right to revoke the DNRO at any time. This can be done verbally or in writing.
- Legal Protection: Healthcare providers are legally protected when they follow the instructions outlined in a valid DNRO.
- Emergency Situations: In emergencies, first responders must have access to the DNRO to ensure compliance with the patient's wishes.
- State Requirements: Familiarize yourself with Florida's specific regulations regarding the DNRO to ensure compliance.
- Communication: Open discussions with family members and healthcare proxies about the DNRO can prevent confusion and ensure everyone's understanding of the patient's wishes.
By keeping these points in mind, individuals can navigate the process of completing and utilizing the Florida Do Not Resuscitate Order form more effectively.
Similar forms
- Living Will: A living will outlines an individual's preferences for medical treatment in situations where they cannot communicate their wishes. Like a DNR, it focuses on end-of-life care but may cover a broader range of medical decisions.
- Durable Power of Attorney for Health Care: This document designates a person to make health care decisions on behalf of someone else. It complements a DNR by ensuring that someone trusted can advocate for the individual's wishes when they cannot do so themselves.
- Advance Directive: An advance directive combines both a living will and a durable power of attorney. It provides guidance on medical treatment preferences and appoints someone to make decisions, similar to how a DNR specifies resuscitation wishes.
- Physician Orders for Life-Sustaining Treatment (POLST): A POLST form translates a patient's wishes into actionable medical orders. Like a DNR, it is designed for individuals with serious illnesses and ensures their preferences are honored in emergencies.
- Health Care Proxy: This document allows a person to appoint someone else to make medical decisions for them. It works alongside a DNR by ensuring that the appointed individual understands and respects the patient's resuscitation preferences.
- Do Not Intubate (DNI) Order: A DNI order specifies that a patient should not be intubated if they stop breathing. Similar to a DNR, it addresses specific life-sustaining measures that the patient wishes to avoid.
- Comfort Care Order: This document emphasizes providing comfort and pain relief rather than aggressive treatment. Like a DNR, it focuses on the quality of life and respects the patient's desire for a peaceful passing.
- Medication Management Plan: This plan outlines how medications should be administered or withheld, especially in end-of-life care. It aligns with a DNR by ensuring that treatment aligns with the patient’s overall care goals.
- Emergency Medical Services (EMS) Do Not Resuscitate (DNR) Form: This specific form is recognized by EMS personnel and provides clear instructions not to perform resuscitation. It is a more formalized version of a DNR that ensures immediate recognition in emergencies.
- Georgia WC 102B Form: This important document acts as a formal notice of representation for parties involved in workers' compensation cases, ensuring proper communication with the State Board of Workers' Compensation. For more information, refer to the Georgia PDF.
- Patient's Bill of Rights: While not a direct counterpart, this document outlines a patient's rights regarding medical treatment and decision-making. It supports the principles behind a DNR by emphasizing the importance of patient autonomy and informed consent.
Misconceptions
Understanding the Florida Do Not Resuscitate Order (DNRO) form is crucial for individuals and families making end-of-life decisions. However, several misconceptions can lead to confusion. Here are six common misunderstandings:
- Misconception 1: The DNRO is the same as a living will.
- Misconception 2: A DNRO means no medical care at all.
- Misconception 3: The DNRO must be signed by a lawyer.
- Misconception 4: A DNRO is permanent and cannot be changed.
- Misconception 5: Healthcare providers must follow a DNRO in all situations.
- Misconception 6: A DNRO is only for terminally ill patients.
The DNRO specifically addresses resuscitation efforts, while a living will outlines broader healthcare decisions. They serve different purposes.
A DNRO only indicates that a person does not want resuscitation in the event of cardiac arrest. Other medical treatments can still be provided.
A DNRO does not require legal representation. It must be completed and signed by a physician and the patient or their legal representative.
Individuals can revoke or modify their DNRO at any time, provided they follow the proper procedures for doing so.
Healthcare providers are required to honor a DNRO only in emergency situations where resuscitation is needed. In non-emergency scenarios, other treatments may still be administered.
Anyone can complete a DNRO, regardless of their health status. It is a personal choice based on individual values and preferences regarding end-of-life care.
Fill out Popular Do Not Resuscitate Order Forms for Specific States
Dnr Form California - Community resources are often available to help patients and families navigate DNR orders and associated discussions.
In New York, utilizing a Bill of Sale is crucial for ensuring that both parties are protected during the transfer of ownership, and for those looking for a reliable resource, NY PDF Forms offers a convenient and accessible way to obtain this important document.
PDF Details
| Fact Name | Description |
|---|---|
| Definition | The Florida Do Not Resuscitate Order (DNRO) form allows individuals to refuse resuscitation efforts in the event of cardiac or respiratory arrest. |
| Governing Law | This form is governed by Florida Statutes, specifically Section 401.45. |
| Eligibility | Any adult individual can complete a DNRO, provided they are of sound mind. |
| Signature Requirement | The form must be signed by the individual or their legally authorized representative. |
| Healthcare Provider's Role | A physician must sign the form to validate the DNRO, ensuring it aligns with the patient’s wishes. |
| Availability | The DNRO form can be obtained online or through healthcare providers and must be printed on bright yellow paper. |
| Revocation | Individuals can revoke the DNRO at any time, and doing so should be communicated to their healthcare provider. |
| Emergency Services | Emergency medical services (EMS) must honor a valid DNRO presented at the scene. |
| Limitations | The DNRO only applies to resuscitation efforts and does not affect other medical treatments or care. |
| Public Awareness | Education about the DNRO is encouraged to help individuals make informed decisions regarding their end-of-life care. |
Documents used along the form
In Florida, the Do Not Resuscitate (DNR) Order form is an important document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. Alongside this form, several other documents are often utilized to ensure that a person's healthcare preferences are respected. Below is a list of common forms and documents that may accompany the Florida DNR Order.
- Advance Directive: This document outlines a person's healthcare preferences, including decisions about medical treatments and appointing a healthcare surrogate to make decisions on their behalf if they become unable to do so.
- Living Will: A specific type of advance directive, a living will details a person's wishes regarding end-of-life care, particularly in situations where they are terminally ill or in a persistent vegetative state.
- Healthcare Surrogate Designation: This form allows an individual to designate someone to make healthcare decisions for them when they are unable to communicate their wishes due to illness or incapacity.
- Physician Orders for Life-Sustaining Treatment (POLST): This document translates a patient's wishes regarding life-sustaining treatment into actionable medical orders that healthcare providers must follow.
- Motorcycle Bill of Sale Form: To properly document your motorcycle transactions, refer to the official motorcycle bill of sale form guide for compliance and accurate ownership transfer.
- Power of Attorney for Healthcare: This legal document grants a designated individual the authority to make healthcare decisions on behalf of another person, particularly if they are unable to make those decisions themselves.
- Do Not Intubate (DNI) Order: Similar to a DNR, this order specifically states that a patient should not be intubated, which means they should not receive assistance with breathing through a tube if they stop breathing.
- Organ Donation Consent: This document expresses an individual's wishes regarding organ donation after death, ensuring that their preferences are honored in the event of their passing.
- Emergency Medical Services (EMS) Protocols: These are guidelines that emergency medical personnel follow, which may include instructions related to DNR orders and other advance directives during emergencies.
- Patient Information Form: This form collects essential information about a patient, including medical history and current medications, which can help healthcare providers make informed decisions in emergencies.
Understanding these documents is crucial for anyone looking to ensure that their healthcare preferences are honored. Each form serves a unique purpose, and together they create a comprehensive approach to managing healthcare decisions, particularly in critical situations. By being informed about these options, individuals can make empowered choices that reflect their values and wishes.