Get Medication Administration Record Sheet Form
Key takeaways
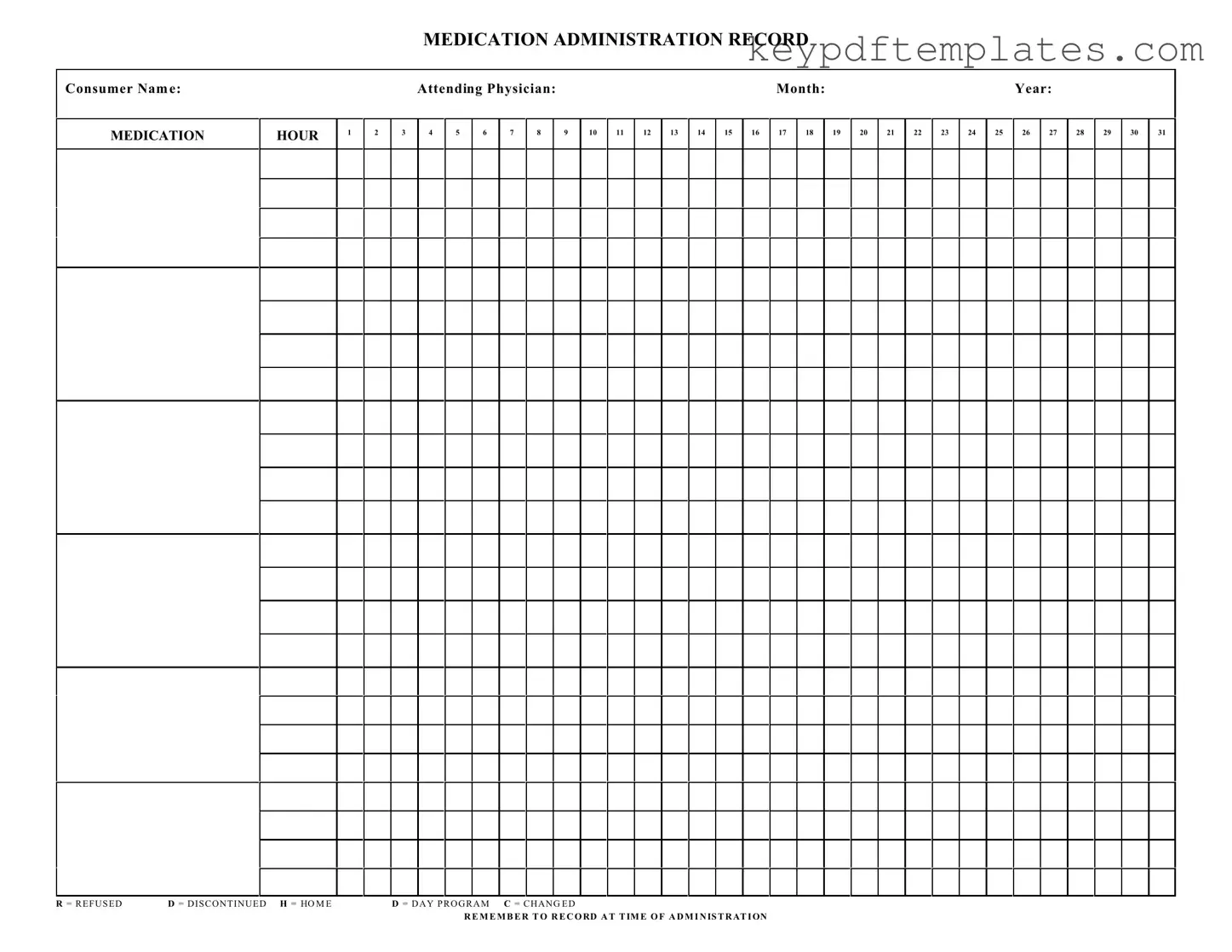
When using the Medication Administration Record Sheet, it’s essential to follow certain guidelines to ensure accuracy and compliance. Here are five key takeaways to keep in mind:
- Complete Consumer Information: Always start by filling in the consumer's name and the attending physician's name. This information is crucial for proper identification and accountability.
- Accurate Date and Time: Record the month and year clearly. Make sure to document the time of administration accurately. This helps in tracking medication schedules effectively.
- Use of Codes: Familiarize yourself with the codes used on the form, such as R for Refused, D for Discontinued, and H for Home. These codes help in maintaining clarity regarding the status of each medication.
- Daily Tracking: The form allows for daily tracking of medication administration. Ensure that you mark each hour appropriately to reflect when medications are given.
- Record Changes Promptly: If there are any changes to the medication plan, such as dosage or frequency, note these immediately on the record. This ensures that everyone involved is informed and can provide consistent care.
Similar forms
-
Patient Care Plan: This document outlines the overall care strategy for a patient, detailing their medical needs, goals, and interventions. Similar to the Medication Administration Record (MAR), it tracks specific actions taken to meet the patient's health requirements.
-
Medication Reconciliation Form: This form is used to ensure that a patient’s medication list is accurate and complete. Like the MAR, it involves careful documentation of medications, including dosages and administration times.
-
Nursing Notes: These notes provide a record of a patient's condition and the care provided. They share a common purpose with the MAR in that both documents are used to communicate important information about medication administration and patient response.
-
Vital Signs Record: This document tracks a patient’s vital signs over time. Both the Vital Signs Record and the MAR serve to monitor patient health, although they focus on different aspects of care.
-
Incident Report: An incident report documents any unusual occurrences during patient care. While the MAR focuses on medication administration, both documents aim to ensure patient safety and quality of care.
-
Treatment Administration Record: This record details the administration of various treatments, similar to how the MAR documents medication. Both forms help ensure that patients receive the correct interventions at the right times.
- Vehicle Purchase Agreement: This form is essential for documenting the sale of a vehicle and ensuring that all terms are clearly stated. For more details, view the document.
-
Discharge Summary: This document summarizes a patient’s care and treatment upon discharge. Like the MAR, it includes critical information about medications and follow-up care, ensuring continuity of care after leaving a healthcare facility.
-
Allergy Record: This document lists any known allergies a patient has. Both the Allergy Record and the MAR are essential for preventing adverse reactions during medication administration.
-
Consent Form: A consent form is used to obtain permission from a patient for specific treatments or medications. Similar to the MAR, it plays a crucial role in ensuring that patients are informed and agree to their care plans.
Misconceptions
Understanding the Medication Administration Record Sheet (MARS) is crucial for ensuring proper medication management. However, several misconceptions can lead to confusion. Here are eight common misconceptions:
- The MARS is only for nurses. Many believe that only nurses can fill out the MARS. In reality, any trained staff member responsible for medication administration can use this form.
- It is optional to record refusals. Some think that recording when a medication is refused is optional. In fact, documenting refusals is essential for tracking patient compliance and safety.
- Only medications prescribed by a physician need to be recorded. This is incorrect. All medications, including over-the-counter drugs and supplements, should be documented on the MARS.
- The MARS does not need to be updated if a medication is changed. This misconception can lead to errors. Any changes in medication must be recorded immediately to ensure accuracy.
- Recording the time of administration is not important. Some may underestimate the significance of timing. Accurate time recording helps monitor medication effectiveness and adherence.
- The MARS is only relevant during the day program. This is misleading. The MARS is important for all settings, including home care and night shifts.
- Once the MARS is filled out, it does not need to be reviewed. This belief can lead to oversights. Regular reviews of the MARS are necessary to ensure ongoing accuracy and compliance.
- All staff members are equally trained to use the MARS. Not all staff may have the same level of training. Ensuring that only trained personnel handle the MARS is vital for patient safety.
By addressing these misconceptions, organizations can enhance their medication administration processes and improve patient care outcomes.
More PDF Templates
Free Voucher - Unlock endless possibilities with our gift certificate.
Da Form 31 Example - Supervisors or approving authorities must sign off on requests.
Having a Georgia Durable Power of Attorney form helps in planning for unforeseen circumstances; it is crucial to ensure that your affairs are managed according to your wishes. For more details about this essential document, visit Georgia PDF.
Faa Form 8050-2 - This bill of sale can be used for various types of aircraft, including planes and helicopters.
Form Specs
| Fact Name | Description |
|---|---|
| Purpose | The Medication Administration Record (MAR) is used to document the administration of medications to consumers. |
| Consumer Information | The form requires the consumer's name and the attending physician's name for accurate record-keeping. |
| Time Tracking | It includes a section to track medication administration by hour, ensuring timely dosages. |
| Month and Year | The form specifies the month and year, which aids in organizing records chronologically. |
| State Regulations | In many states, the use of MAR forms is governed by healthcare regulations, such as those outlined in the Nurse Practice Act. |
| Medication Status Codes | Abbreviations like R (Refused), D (Discontinued), and H (Home) help clarify the status of each medication entry. |
| Documentation Reminder | The form includes a reminder to record administration at the time it occurs, promoting accuracy in documentation. |
Documents used along the form
The Medication Administration Record Sheet is a vital document in healthcare settings, specifically for tracking the administration of medications to patients. Several other forms and documents often accompany this record to ensure comprehensive patient care and accurate documentation. Below is a list of these related documents.
- Patient Intake Form: This document collects essential information about the patient, including personal details, medical history, and current medications. It serves as the foundation for patient care.
- Medication Order Form: This form is used by healthcare providers to prescribe medications. It includes details such as the medication name, dosage, route of administration, and duration of therapy.
- Allergy Information Form: This document records any known allergies the patient may have. It is crucial for preventing adverse reactions during medication administration.
- Consent for Treatment Form: Patients sign this form to give permission for medical treatments, including medication administration. It ensures that patients are informed about the procedures they will undergo.
- Medication Reconciliation Form: This form is used to compare a patient's current medication list with new medications being prescribed. It helps to avoid medication errors and ensures continuity of care.
- Incident Report Form: If an adverse event occurs during medication administration, this form documents the incident. It is essential for quality improvement and patient safety initiatives.
- Patient Education Materials: These documents provide information about medications, including potential side effects and instructions for use. They empower patients to participate in their own care.
- Texas Form: The Texas form, a crucial document required for various legal and administrative processes within the state, serves as an official means to submit necessary information. For a seamless experience, ensure you have all the relevant details ready before you start. More information can be found at txtemplate.com/texas-pdf-template/.
- Nursing Notes: Nurses document observations and actions related to patient care in this form. It includes notes on medication administration, patient responses, and any changes in condition.
- Discharge Summary: This document outlines the patient's care during their stay, including medications prescribed at discharge. It ensures that patients have a clear understanding of their ongoing treatment.
These forms and documents work together to enhance patient safety and ensure effective communication among healthcare providers. Proper documentation is essential for delivering high-quality care and maintaining compliance with regulatory standards.