Get Progress Notes Form
Key takeaways
When filling out and using the Progress Notes form, keep these key takeaways in mind:
- Accurate Patient Identification: Always provide complete and correct patient information. This includes the patient's name (last, first, middle), grade, rank, rate, and the medical facility's name.
- Consistent Date Entry: Ensure that the date is clearly marked on the form. This helps maintain an accurate timeline of the patient's medical history and treatment.
- Use Standard Format: Follow the structure outlined in the Standard Form 509. Adhering to this format ensures clarity and uniformity across medical records.
- Review for Completeness: Before submitting the form, double-check that all sections are filled out completely. Incomplete entries can lead to misunderstandings in patient care.
Similar forms
The Progress Notes form shares similarities with several other documents used in medical and healthcare settings. Below is a list of nine documents that have comparable features:
- Patient Encounter Form: Like Progress Notes, this form records details about patient visits, including symptoms, treatments, and follow-up care.
- SOAP Notes: Both documents use a structured format to document patient information, focusing on Subjective, Objective, Assessment, and Plan.
- Medical History Form: This form collects comprehensive patient history, similar to how Progress Notes summarize ongoing treatment and patient progress.
- Discharge Summary: Both documents provide a summary of care, with Discharge Summaries detailing the patient’s hospital stay and Progress Notes tracking treatment over time.
- Referral Form: This document, like Progress Notes, includes patient identification and details about the reason for referral, ensuring continuity of care.
- Treatment Plan: Both documents outline treatment strategies, with Treatment Plans focusing on long-term goals while Progress Notes track daily or weekly progress.
- Clinical Assessment Form: Similar to Progress Notes, this form evaluates patient conditions and progress, often used in conjunction with ongoing treatment documentation.
- General Power of Attorney: This essential form in Georgia allows an individual to make important decisions on behalf of another person, ensuring that their legal and financial affairs are managed according to their wishes. For more information, visit Georgia PDF.
- Medication Administration Record (MAR): Both track patient care, with MAR focusing specifically on medications administered, while Progress Notes encompass broader patient interactions.
- Case Management Notes: These notes document interactions and plans for patient care, paralleling the ongoing updates found in Progress Notes.
Misconceptions
Progress Notes forms are essential tools in the medical field, yet several misconceptions often arise regarding their purpose and use. Understanding these misconceptions can help clarify their importance and improve patient care. Below are seven common misconceptions about the Progress Notes form, along with explanations to dispel them.
- Progress Notes are optional. Many believe that documenting progress notes is a discretionary task. In reality, these notes are a critical component of patient care, ensuring continuity and communication among healthcare providers.
- Progress Notes are only for doctors. While physicians frequently complete these notes, they are also utilized by nurses, therapists, and other healthcare professionals. Everyone involved in patient care contributes to and benefits from accurate documentation.
- Progress Notes are only for serious cases. Some may think that progress notes are necessary only for complex or severe conditions. However, documenting even routine visits is vital for tracking patient history and treatment effectiveness.
- Progress Notes can be vague. There is a misconception that progress notes do not need to be detailed. In fact, clear and specific documentation is essential. Vague notes can lead to misunderstandings and compromise patient safety.
- Progress Notes are only for legal purposes. While documentation can serve as legal evidence, the primary purpose of progress notes is to facilitate patient care. They help providers make informed decisions based on a patient's history and treatment progress.
- Progress Notes are only relevant during a patient's visit. Some individuals believe that progress notes are only important while a patient is in the facility. However, these notes provide valuable information for future visits and ongoing treatment.
- Progress Notes can be completed after the patient leaves. There is a common belief that notes can be filled out at any time. Ideally, progress notes should be completed during or immediately after the patient encounter to ensure accuracy and comprehensiveness.
Addressing these misconceptions can enhance the understanding of the Progress Notes form, ultimately leading to better patient outcomes and improved healthcare practices.
More PDF Templates
Fake Utility Bill Generator - Application form for low-income utility programs.
Ncoer Support Form Fillable - The NCO evaluation report is a crucial component of professional development.
The Chick Fil A Job Application form serves as the first step for prospective employees to express their interest in joining the renowned fast-food chain. This document gathers essential personal, educational, and professional information required for employment consideration. To begin the application process, applicants can print and complete the form, making it a crucial bridge connecting job seekers with potential employment opportunities at Chick Fil A.
Why Would a Court Case Be Continued - A formal application to change the hearing date.
Form Specs
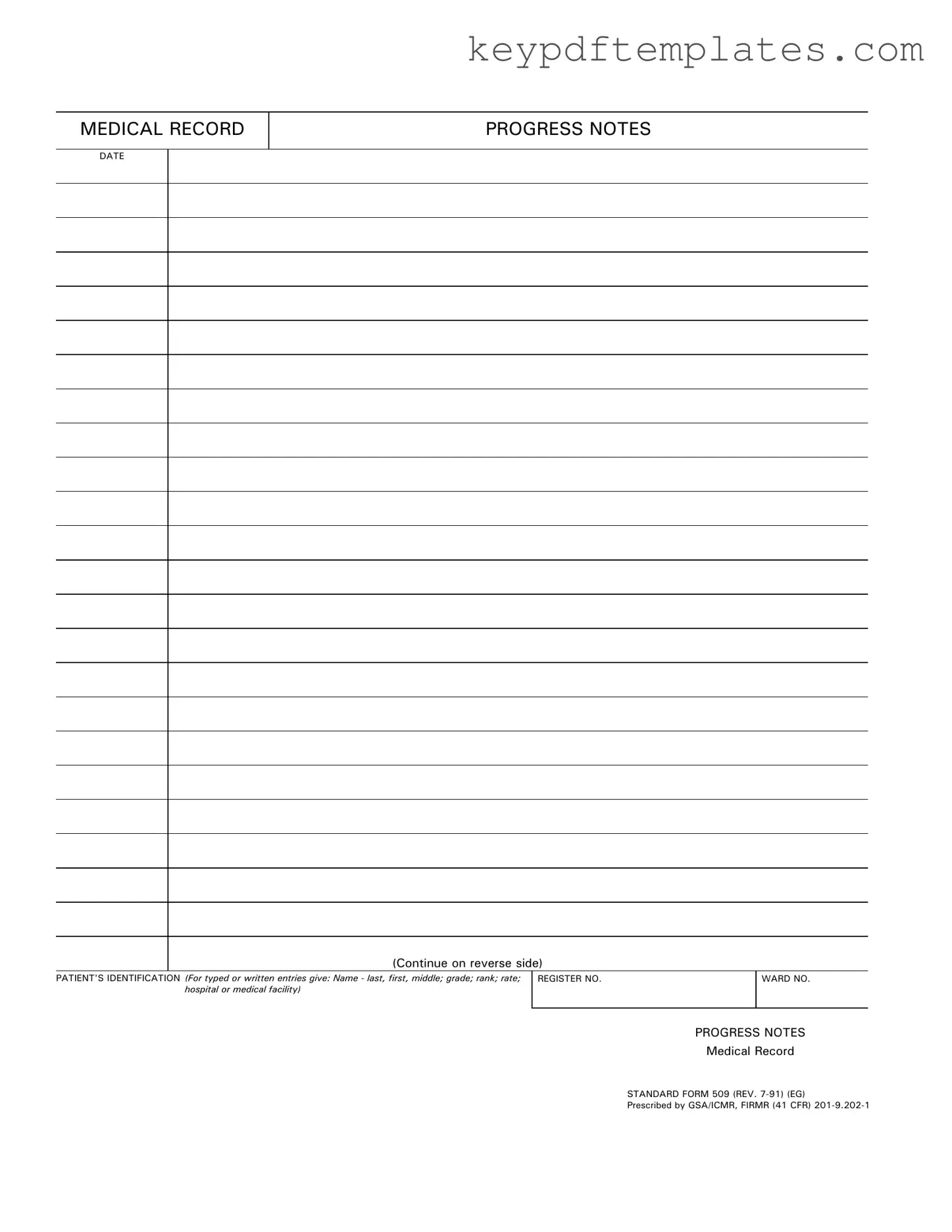
| Fact Name | Description |
|---|---|
| Form Purpose | The Progress Notes form is used to document patient care and treatment updates in medical records. |
| Identification Requirements | It requires the patient's identification, including name, grade, rank, rate, and the medical facility. |
| Standardization | This form is a standardized document, specifically Standard Form 509, revised in July 1991. |
| Governing Laws | It is prescribed by GSA/ICMR and adheres to FIRMR regulations outlined in 41 CFR 201-9.202-1. |
| Usage Continuation | There is a provision to continue notes on the reverse side of the form if more space is needed. |
| Revision History | The form has undergone revisions, with the latest being in July 1991, ensuring it meets current medical documentation standards. |
Documents used along the form
In the realm of healthcare documentation, the Progress Notes form plays a vital role in tracking a patient's journey through treatment. However, it is often accompanied by several other important forms and documents that contribute to a comprehensive medical record. Understanding these documents can enhance the quality of care and ensure that all relevant information is readily available to healthcare providers.
- Admission Assessment Form: This document is completed upon a patient’s entry into a healthcare facility. It gathers essential information about the patient’s medical history, current health status, and any specific needs they may have. This form helps establish a baseline for ongoing care.
- Motor Vehicle Power of Attorney: This important legal document allows an individual to delegate authority to another person for handling motor vehicle transactions, critical for those unable to manage such matters themselves. For more information, visit https://allfloridaforms.com.
- Care Plan: The care plan outlines the specific goals and interventions for a patient’s treatment. It is developed collaboratively by the healthcare team and is updated regularly to reflect changes in the patient's condition or response to treatment.
- Discharge Summary: This document is created when a patient is ready to leave the healthcare facility. It summarizes the patient's treatment, progress, and any follow-up care needed. The discharge summary ensures continuity of care as the patient transitions back to their home or another setting.
- Medication Administration Record (MAR): The MAR is a critical document that tracks all medications administered to a patient during their stay. It includes details such as dosage, frequency, and any adverse reactions. This record is essential for ensuring patient safety and effective medication management.
Each of these documents serves a unique purpose and collectively enhances the quality of patient care. By familiarizing oneself with these forms, healthcare professionals can ensure that they are providing thorough and informed care to their patients.